Page 17 - Work Force April 2020
P. 17
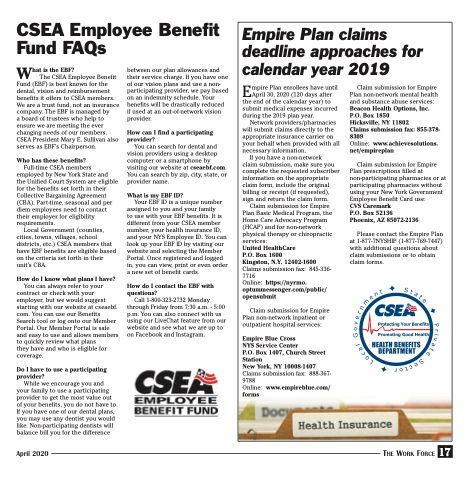
CSEA Employee Benefit Fund FAQs
Empire Plan claims deadline approaches for calendar year 2019
Empire Plan enrollees have until April 30, 2020 (120 days after the end of the calendar year) to submit medical expenses incurred during the 2019 plan year.
Network providers/pharmacies will submit claims directly to the appropriate insurance carrier on your behalf when provided with all necessary information.
If you have a non-network
claim submission, make sure you complete the requested subscriber information on the appropriate claim form, include the original billing or receipt (if requested), sign and return the claim form.
Claim submission for Empire Plan Basic Medical Program, the Home Care Advocacy Program (HCAP) and for non-network physical therapy or chiropractic services:
United HealthCare
P.O. Box 1600
Kingston, N.Y. 12402-1600 Claims submission fax: 845-336- 7716
Online: https://nyrmo. optummessenger.com/public/ opensubmit
Claim submission for Empire Plan non-network inpatient or outpatient hospital services:
Empire Blue Cross
NYS Service Center
P.O. Box 1407, Church Street Station
New York, NY 10008-1407 Claims submission fax: 888-367- 9788
Online: www.empireblue.com/ forms
Claim submission for Empire Plan non-network mental health and substance abuse services: Beacon Health Options, Inc. P.O. Box 1850
Hicksville, NY 11802
Claims submission fax: 855-378- 8309
Online: www.achievesolutions. net/empireplan
Claim submission for Empire Plan prescriptions filled at non-participating pharmacies or at participating pharmacies without using your New York Government Employee Benefit Card use:
CVS Caremark
P.O. Box 52136 Phoenix, AZ 85072-2136
Please contact the Empire Plan at 1-877-7NYSHIP (1-877-769-7447) with additional questions about claim submissions or to obtain claim forms.
What is the EBF?
The CSEA Employee Benefit Fund (EBF) is best known for the
dental, vision and reimbursement benefits it offers to CSEA members. We are a trust fund, not an insurance company. The EBF is managed by
a board of trustees who help to ensure we are meeting the ever changing needs of our members. CSEA President Mary E. Sullivan also serves as EBF’s Chairperson.
Who has these benefits?
Full-time CSEA members employed by New York State and the Unified Court System are eligible for the benefits set forth in their Collective Bargaining Agreement (CBA). Part-time, seasonal and per diem employees need to contact their employer for eligibility requirements.
Local Government (counties, cities, towns, villages, school districts, etc.) CSEA members that have EBF benefits are eligible based on the criteria set forth in their unit’s CBA.
How do I know what plans I have?
You can always refer to your contract or check with your employer, but we would suggest starting with our website at cseaebf. com. You can use our Benefits Search tool or log onto our Member Portal. Our Member Portal is safe and easy to use and allows members to quickly review what plans
they have and who is eligible for coverage.
Do I have to use a participating provider?
While we encourage you and your family to use a participating provider to get the most value out of your benefits, you do not have to. If you have one of our dental plans, you may use any dentist you would like. Non-participating dentists will balance bill you for the difference
between our plan allowances and their service charge. If you have one of our vision plans and use a non- participating provider, we pay based on an indemnity schedule. Your benefits will be drastically reduced if used at an out-of-network vision provider.
How can I find a participating provider?
You can search for dental and vision providers using a desktop computer or a smartphone by visiting our website at cseaebf.com. You can search by zip, city, state, or provider name.
What is my EBF ID?
Your EBF ID is a unique number assigned to you and your family
to use with your EBF benefits. It is different from your CSEA member number, your health insurance ID, and your NYS Employee ID. You can look up your EBF ID by visiting our website and selecting the Member Portal. Once registered and logged in, you can view, print or even order a new set of benefit cards.
How do I contact the EBF with questions?
Call 1-800-323-2732 Monday through Friday from 7:30 a.m. - 5:00 p.m. You can also connect with us using our LiveChat feature from our website and see what we are up to on Facebook and Instagram.
April 2020
The Work Force 17