Page 17 - Work Force January 2020
P. 17
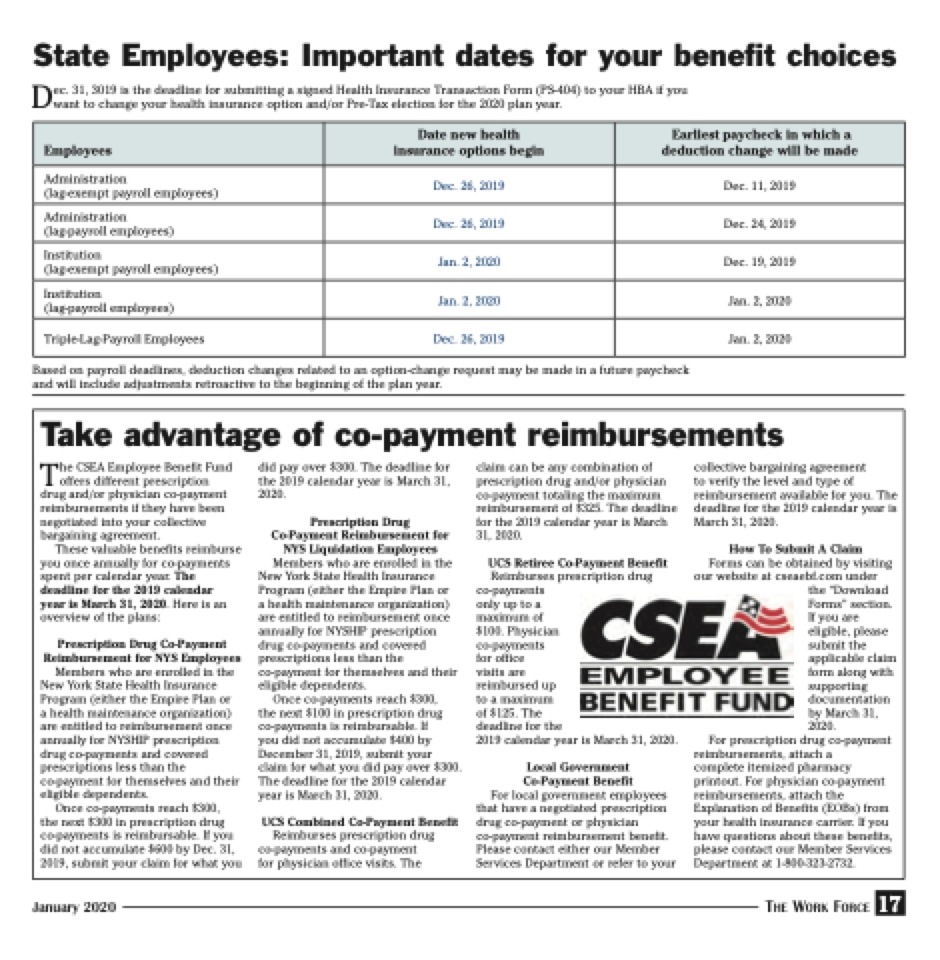
State Employees: Important dates for your benefit choices
Dec. 31, 3019 is the deadline for submitting a signed Health Insurance Transaction Form (PS-404) to your HBA if you want to change your health insurance option and/or Pre-Tax election for the 2020 plan year.
Employees
Date new health insurance options begin
Earliest paycheck in which a deduction change will be made
Administration
(lag-exempt payroll employees)
Dec. 26, 2019
Dec. 11, 2019
Administration (lag-payroll employees)
Dec. 26, 2019
Dec. 24, 2019
Institution
(lag-exempt payroll employees)
Jan. 2, 2020
Dec. 19, 2019
Institution
(lag-payroll employees)
Jan. 2, 2020
Jan. 2, 2020
Triple-Lag-Payroll Employees
Dec. 26, 2019
Jan. 2, 2020
Based on payroll deadlines, deduction changes related to an option-change request may be made in a future paycheck and will include adjustments retroactive to the beginning of the plan year.
Take advantage of co-payment reimbursements
The CSEA Employee Benefit Fund offers different prescription drug and/or physician co-payment reimbursements if they have been negotiated into your collective bargaining agreement.
These valuable benefits reimburse you once annually for co-payments spent per calendar year. The deadline for the 2019 calendar
year is March 31, 2020. Here is an overview of the plans:
Prescription Drug Co-Payment Reimbursement for NYS Employees
Members who are enrolled in the New York State Health Insurance Program (either the Empire Plan or a health maintenance organization) are entitled to reimbursement once annually for NYSHIP prescription drug co-payments and covered prescriptions less than the co-payment for themselves and their eligible dependents.
Once co-payments reach $300,
the next $300 in prescription drug co-payments is reimbursable. If you did not accumulate $600 by Dec. 31, 2019, submit your claim for what you
did pay over $300. The deadline for the 2019 calendar year is March 31, 2020.
Prescription Drug Co-Payment Reimbursement for NYS Liquidation Employees
Members who are enrolled in the New York State Health Insurance Program (either the Empire Plan or a health maintenance organization) are entitled to reimbursement once annually for NYSHIP prescription drug co-payments and covered prescriptions less than the co-payment for themselves and their eligible dependents.
Once co-payments reach $300,
the next $100 in prescription drug co-payments is reimbursable. If
you did not accumulate $400 by December 31, 2019, submit your claim for what you did pay over $300. The deadline for the 2019 calendar year is March 31, 2020.
UCS Combined Co-Payment Benefit
Reimburses prescription drug co-payments and co-payment for physician office visits. The
claim can be any combination of prescription drug and/or physician co-payment totaling the maximum reimbursement of $325. The deadline for the 2019 calendar year is March 31, 2020.
UCS Retiree Co-Payment Benefit
Reimburses prescription drug co-payments
only up to a
maximum of
$100. Physician
co-payments
for office
visits are
reimbursed up
to a maximum
of $125. The
deadline for the
2019 calendar year is March 31, 2020.
Local Government Co-Payment Benefit
For local government employees
that have a negotiated prescription drug co-payment or physician co-payment reimbursement benefit. Please contact either our Member Services Department or refer to your
collective bargaining agreement
to verify the level and type of reimbursement available for you. The deadline for the 2019 calendar year is March 31, 2020.
How To Submit A Claim
Forms can be obtained by visiting our website at cseaebf.com under
the “Download Forms” section. If you are eligible, please submit the applicable claim form along with supporting documentation by March 31, 2020.
For prescription drug co-payment reimbursements, attach a
complete itemized pharmacy printout. For physician co-payment reimbursements, attach the Explanation of Benefits (EOBs) from your health insurance carrier. If you have questions about these benefits, please contact our Member Services Department at 1-800-323-2732.
January 2020 The Work Force 17