Page 17 - Work Force July-August 2025
P. 17
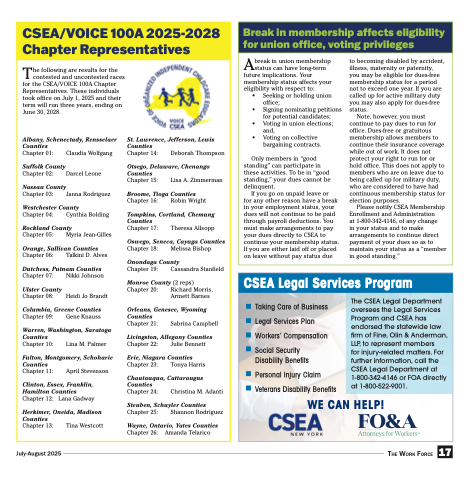
CSEA/VOICE 100A 2025-2028 Chapter Representatives
The following are results for the contested and uncontested races for the CSEA/VOICE 100A Chapter Representatives. These individuals took office on July 1, 2025 and their term will run three years, ending on June 30, 2028.
Albany, Schenectady, Rensselaer
St. Lawrence, Jefferson, Lewis Counties
Chapter 14: Deborah Thompson
Otsego, Delaware, Chenango Counties
Chapter 15: Lisa A. Zimmerman
Broome, Tioga Counties
Chapter 16: Robin Wright
Tompkins, Cortland, Chemung Counties
Chapter 17: Theresa Allsopp
Oswego, Seneca, Cayuga Counties
Chapter 18: Melissa Bishop
Onondaga County
Chapter 19: Cassandra Stanfield
Monroe County (2 reps) Chapter 20: Richard Morris,
Armett Barnes
Orleans, Genesee, Wyoming Counties
Chapter 21: Sabrina Campbell
Livingston, Allegany Counties
Chapter 22: Julie Bennett
Erie, Niagara Counties
Chapter 23: Tonya Harris
Chautauqua, Cattaraugus Counties
Chapter 24: Christina M. Adanti
Steuben, Schuyler Counties
Chapter 25: Shannon Rodriguez
Wayne, Ontario, Yates Counties
Chapter 26: Amanda Telarico
Counties
Chapter 01:
Suffolk County
Chapter 02:
Claudia Wolfgang Darcel Leone
Nassau County
Chapter 03: Janna Rodriguez
Westchester County
Chapter 04: Cynthia Bolding
Rockland County
Chapter 05: Myria Jean-Gilles
Orange, Sullivan Counties
Chapter 06: Talkini D. Alves
Dutchess, Putnam Counties
Chapter 07:
Ulster County
Chapter 08:
Nikki Johnson Heidi Jo Brandt
Columbia, Greene Counties
Chapter 09: Gene Knauss
Warren, Washington, Saratoga Counties
Chapter 10: Lina M. Palmer
Fulton, Montgomery, Schoharie Counties
Chapter 11: April Stevenson
Clinton, Essex, Franklin, Hamilton Counties Chapter 12: Lana Gadway
Herkimer, Oneida, Madison Counties
Chapter 13: Tina Westcott
Break in membership affects eligibility for union office, voting privileges
Abreak in union membership status can have long-term future implications. Your membership status affects your eligibility with respect to:
• Seeking or holding union office;
• Signing nominating petitions for potential candidates;
• Voting in union elections; and,
• Voting on collective bargaining contracts.
Only members in “good standing” can participate in these activities. To be in “good standing,” your dues cannot be delinquent.
If you go on unpaid leave or
for any other reason have a break in your employment status, your dues will not continue to be paid through payroll deductions. You must make arrangements to pay your dues directly to CSEA to continue your membership status. If you are either laid off or placed on leave without pay status due
to becoming disabled by accident, illness, maternity or paternity, you may be eligible for dues-free membership status for a period not to exceed one year. If you are called up for active military duty you may also apply for dues-free status.
Note, however, you must continue to pay dues to run for office. Dues-free or gratuitous membership allows members to continue their insurance coverage while out of work. It does not protect your right to run for or hold office. This does not apply to members who are on leave due to being called up for military duty, who are considered to have had continuous membership status for election purposes.
Please notify CSEA Membership Enrollment and Administration
at 1-800-342-4146, of any change
in your status and to make arrangements to continue direct payment of your dues so as to maintain your status as a “member in good standing.”
CSEA Legal Services Program
Taking Care of Business
Legal Services Plan
Workers’ Compensation
Social Security Disability Benefits
Personal Injury Claim Veterans Disability Benefits
WE CAN HELP!
The CSEA Legal Department oversees the Legal Services Program and CSEA has endorsed the statewide law firm of Fine, Olin & Anderman, LLP, to represent members
for injury-related matters. For further information, call the CSEA Legal Department at 1-800-342-4146 or FOA directly at 1-800-522-9001.
July-August 2025 The Work Force 17