Page 17 - Work Force October 2022
P. 17
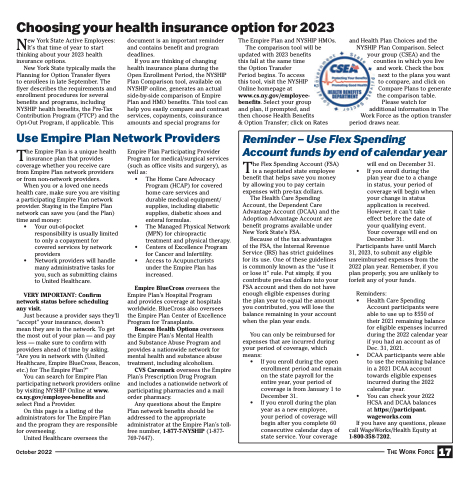
Choosing your health insurance option for 2023
New York State Active Employees: It’s that time of year to start thinking about your 2023 health insurance options.
New York State typically mails the Planning for Option Transfer flyers
to enrollees in late September. The flyer describes the requirements and enrollment procedures for several benefits and programs, including NYSHIP health benefits, the Pre-Tax Contribution Program (PTCP) and the Opt-Out Program, if applicable. This
document is an important reminder and contains benefit and program deadlines.
If you are thinking of changing health insurance plans during the Open Enrollment Period, the NYSHIP Plan Comparison tool, available on NYSHIP online, generates an actual side-by-side comparison of Empire Plan and HMO benefits. This tool can help you easily compare and contrast services, copayments, coinsurance amounts and special programs for
The Empire Plan and NYSHIP HMOs. The comparison tool will be
updated with 2023 benefits
this fall at the same time
the Option Transfer
Period begins. To access
this tool, visit the NYSHIP
Online homepage at www.cs.ny.gov/employee- benefits. Select your group
and plan, if prompted, and
then choose Health Benefits
& Option Transfer; click on Rates
and Health Plan Choices and the NYSHIP Plan Comparison. Select
your group (CSEA) and the counties in which you live and work. Check the box
next to the plans you want to compare, and click on Compare Plans to generate
the comparison table. Please watch for
additional information in The Work Force as the option transfer
period draws near.
Use Empire Plan Network Providers
Reminder – Use Flex Spending Account funds by end of calendar year
The Flex Spending Account (FSA) is a negotiated state employee benefit that helps save you money by allowing you to pay certain expenses with pre-tax dollars.
The Health Care Spending Account, the Dependent Care Advantage Account (DCAA) and the Adoption Advantage Account are benefit programs available under New York State’s FSA.
Because of the tax advantages of the FSA, the Internal Revenue Service (IRS) has strict guidelines for its use. One of these guidelines is commonly known as the “use it or lose it” rule. Put simply, if you contribute pre-tax dollars into your FSA account and then do not have enough eligible expenses during the plan year to equal the amount you contributed, you will lose the balance remaining in your account when the plan year ends.
You can only be reimbursed for expenses that are incurred during your period of coverage, which means:
• If you enroll during the open enrollment period and remain on the state payroll for the entire year, your period of coverage is from January 1 to December 31.
• If you enroll during the plan year as a new employee, your period of coverage will begin after you complete 60 consecutive calendar days of state service. Your coverage
will end on December 31. • If you enroll during the
plan year due to a change in status, your period of coverage will begin when your change in status application is received. However, it can’t take effect before the date of your qualifying event. Your coverage will end on December 31.
Participants have until March 31, 2023, to submit any eligible unreimbursed expenses from the 2022 plan year. Remember, if you plan properly, you are unlikely to forfeit any of your funds.
Reminders:
• Health Care Spending
Account participants were able to use up to $550 of their 2021 remaining balance for eligible expenses incurred during the 2022 calendar year if you had an account as of Dec. 31, 2021.
• DCAA participants were able to use the remaining balance in a 2021 DCAA account towards eligible expenses incurred during the 2022 calendar year.
• You can check your 2022 HCSA and DCAA balances at https://par ticipant. wageworks.com
If you have any questions, please call WageWorks/Health Equity at 1-800-358-7202.
17
The Empire Plan is a unique health insurance plan that provides coverage whether you receive care from Empire Plan network providers or from non-network providers.
When you or a loved one needs health care, make sure you are visiting a participating Empire Plan network provider. Staying in the Empire Plan network can save you (and the Plan) time and money:
• Your out-of-pocket responsibility is usually limited to only a copayment for covered services by network providers
• Network providers will handle many administrative tasks for you, such as submitting claims to United Healthcare.
VERY IMPORTANT: Confirm network status before scheduling any visit.
Just because a provider says they’ll “accept” your insurance, doesn’t
mean they are in the network. To get the most out of your plan — and pay less — make sure to confirm with providers ahead of time by asking, “Are you in network with (United Healthcare, Empire BlueCross, Beacon, etc.) for The Empire Plan?”
You can search for Empire Plan participating network providers online by visiting NYSHIP Online at www. cs.ny.gov/employee-benefits and select Find a Provider.
On this page is a listing of the administrators for The Empire Plan and the program they are responsible for overseeing.
United Healthcare oversees the
Empire Plan Participating Provider Program for medical/surgical services (such as office visits and surgery), as well as:
• The Home Care Advocacy Program (HCAP) for covered home care services and durable medical equipment/ supplies, including diabetic supplies, diabetic shoes and enteral formulas.
• The Managed Physical Network (MPN) for chiropractic treatment and physical therapy.
• Centers of Excellence Program for Cancer and Infertility.
• Access to Acupuncturists under the Empire Plan has increased.
Empire BlueCross oversees the Empire Plan’s Hospital Program
and provides coverage at hospitals worldwide. BlueCross also oversees the Empire Plan Center of Excellence Program for Transplants.
Beacon Health Options oversees the Empire Plan’s Mental Health and Substance Abuse Program and provides a nationwide network for mental health and substance abuse treatment, including alcoholism.
CVS Caremark oversees the Empire Plan’s Prescription Drug Program
and includes a nationwide network of participating pharmacies and a mail order pharmacy.
Any questions about the Empire Plan network benefits should be addressed to the appropriate administrator at the Empire Plan’s toll- free number, 1-877-7-NYSHIP (1-877- 769-7447).
October 2022
The Work Force